Thin Endometrial Lining
Thin Endometrium- Causes and Treatment
What is endometrium?
The endometrium is the innermost lining layer of the uterus. Every month, the endometrial lining thickens in preparation to receive the embryo and sheds as menses in case there is no pregnancy.
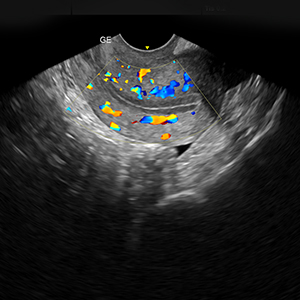
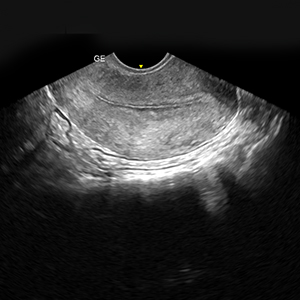
However, in case the egg is fertilized by the sperm, then the endometrium undergoes changes to make a hospitable environment for the embryo to implant, be nourished and grow. A good endometrium is vital to a successful pregnancy. Ideal endometrial lining is one that is >8mm, echogenic and blood-supply rich.
What is thin endometrium? Does it reduce pregnancy rates?
Endometrial thickness is associated with live births in IVF.
An endometrial thickness of less than 7 mm decreases the pregnancy rate In Vitro Fertilization by an odds ratio of 0.4 and the live birth rate in a normal endometrium is halved when the thickness is <5mm.
Few pregnancies, however, have been reported with an endometrial thickness as low as 4 mm. Thin endometrial lining is usually a damaged uterine lining caused by changes in the hormonal levels, reduced blood flow to the uterus and infection, most common being Endometrial Tuberculosis.
What are the signs of thin endometrium?
In most cases, this is a silent symptom. Issues pertaining to thin endometrial lining usually occur for years before the women try to conceive. Most women are unaware of the endometrium problem till they are tested. Some signs that women show are:
Light irregular menses: Women may complain of very light menstrual bleed which may last only half a day.
Infertility: Most of them have trouble falling pregnant or have history of repeated miscarriages.
What are the causes of thin endometrium?
Thin endometrium can result from various factors the most common being inflammatory and iatrogenic. Poor vascularity and low estradiol values can also lead to poor endometrial growth. The endometrium can also be inherently thin in some women.
1) Hormonal: Low estrogen levels or hormonal imbalances can lead to thinning of the uterine lining.
2) Age: There is thinning of the endometrial lining with advancing age, particularly after menopause
3) Inflammatory causes: Infection of the endometrium (Endometritis) can lead to the destruction of the basal layer of the endometrium. Regeneration of endometrium even after complete treatment is very difficult as scar tissue destroys the basal layer.
4) Idiopathic: Thin endometrium can also a result from individual uterine architecture or the intrinsic properties of endometrium that affect its growth. Low estrogen levels as well as reduced blood supply to the uterus can also cause a thin uterine lining.
5) Iatrogenic: Repeated or vigorous curettage can sometimes damage the basal layer of endometrium. Formation of adhesions post laparoscopic surgeries for polypectomy or fibroids as well as use of drugs such as clomiphene citrate can cause thinning of the uterine lining.
What is the treatment for thin endometrial lining?
There are a number of options available to you if you have been diagnosed with a thin endometrial lining. While a number of medication is available to you and your physician will guide you to the best treatment option for you, there are some lifestyle changes which you can incorporate in your daily routine to help you improve the same. Some of these are:
Thin endometrial lining is often due to poor blood circulation. Increasing the physical activity will help improve your blood circulation and this in turn will help thicken your endometrial lining. Body massages help to stimulate the nerves and muscles of our body. When performed by trained massage therapist, it helps to detoxify and strengthen the muscles, improve blood circulation and thus improve the endometrial lining.
A number of herbal supplements are available that help improve Estrogen levels. Thin endometrial lining could be due to lower estrogen levels in the body. Taking supplements rich in phytoestrogens will help improve the hormonal levels. These include maca root and royal jelly. Foods rich in Soya and fruits like grapefruit, apple and strawberry are rich in phytoestrogens. Vitamin E and L-Arginine also help improve the lining.
Platelet Rich Plasma is a rich concentrate of growth factors and platelets obtained from patient’s own blood. These have shown to have a favorable impact on the endometrial receptivity by improving blood flow to the uterus and endometrial lining thickness.
PRP is prepared by drawing patient’s blood and processing it to extract platelets and growth factors. During the procedure the rich concentrate is infused in the uterus using an IUI catheter. The patient rests for 10 mins and can subsequently resume normal daily activities. It is an OPD procedure with no need for anesthesia.
At Corion we offer intrauterine PRP for patients suffering from thin endometrium and patients with recurrent implantation Failure.
Exogenous Estrogen administration in high dosages either as oral tablets, vaginal pessaries, estrogen patches or as transdermal creams when administered for a longer duration (14-18 days) help to improve the endometrial thickness. Your physician will guide you to the best option for you.
This is a day care procedure, performed under short general anesthesia, in which a camera is inserted into the uterine cavity to check if the endometrial lining is good. It is also done to treat any adhesions or removal of scar tissue inside the uterus. It also helps to diagnose presence of any infection.
Need help, Contact Us….
Thin endometrium can be a cause of concern to couples who are trying to conceive. At Corion, our highly qualified doctor team will help you to navigate this issue and overcome this difficulty with ease. Write to us at reachus@corionfertilityclinic.com or call us at 91 912226395599.
OUR SERVICES:
Sperm DNA Fragmentation Ovarian rejuvination Thin Endometrial Lining PGS (PGT-A) & PGD (PGT-M) Cryopreservation / Fertility Preservation / Vitrification Egg Freezing / Oocyte Cryopreservation Sperm Cryopreservation Vitrification & Frozen Embryo Transfer Recurrent Pregnancy Loss IUI-Intrauterine Insemination Blastocyst Transfer Laser Assisted Hatching Follicular Monitoring TESA-Testicular Sperm Extraction PESA – Per Epididymal Sperm AspirationCopyright © 2024, Corion. All Rights Reserved.
Website is designed & developed by Phi Brands


